
Every healthcare organization that employs physician providers, whether it’s a health system or hospital (HSH) or private practice group, determines its own compensation method for its physicians. With the current economic climate putting extreme financial pressure on HSHs, many are looking for new ways to reduce their investment in the employed medical group while also creating incentives to improve the group’s performance.
Below are some key considerations to help you create a physician compensation plan that best meets these goals for your organization.
Until recently, most physicians were in private practice. Now, 70% of physicians are employed and many work for an HSH with projections indicating this trend will only continue to grow. As HSHs aim to refine their physician compensation strategies, many are looking to incorporate aspects that independent practices use to craft their compensation models for support.
Historically, private groups have opted for some form of productivity distribution. They may use provider collections/net revenue, work Relative Value Units (wRVUs) or a variety of other metrics as the basis for compensation.
Which approach a private group uses depends on the nature of the group. A single specialty practice may base pay on the individual’s percentage of total group productivity of the group’s net income available. A multi-specialty practice may allocate the group’s operating expenses against individual physician productivity. Others may divide the income equally among the physicians or combine these basic methods.
The one common factor is the physicians share an economic interest in the overall group’s performance. The example below is of a private medical group that uses an individual percentage of total group productivity method.
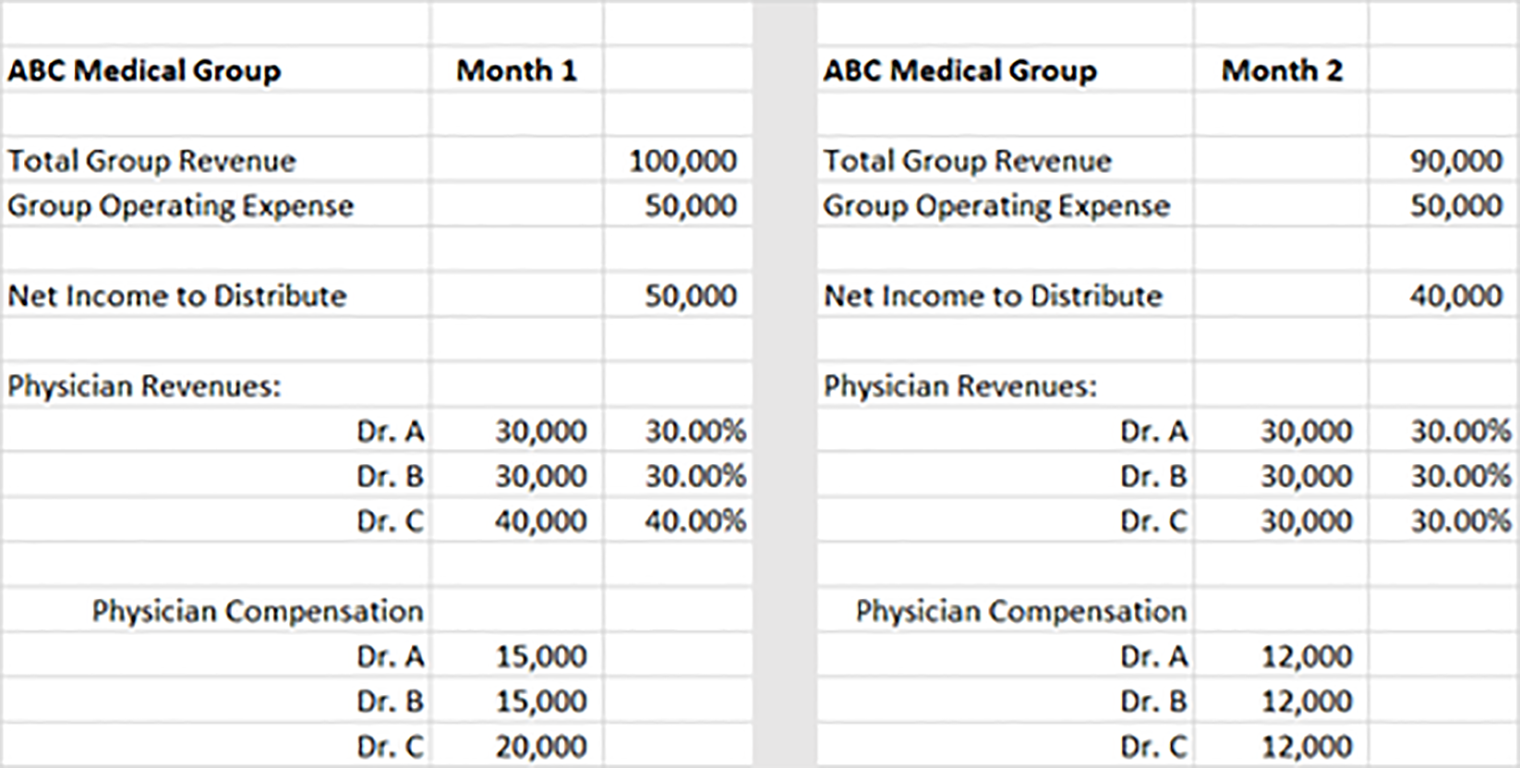
Here, only Dr. C’s revenues decreased in Month 2, but all three doctors saw a reduction in compensation. This shows the effect on all physicians’ income if one member’s productivity declines. The opposite is also true, if one member’s productivity increases, all physicians’ income increases.
HSH physician employment and acquisitions take on many forms, but they typically include:
In most of these employment agreements, the shared economic interest of the physicians isn’t considered. Or in the case of acquisitions, it’s eliminated entirely. This fundamentally changes the peer pressure dynamic within a medical group often seen in private practices. Essentially, HSHs have created a collection of employed physicians and not a traditional medical group.
In fact, many employment and acquisition transactions are negotiated individually and aren’t consistent in approach, even within specialties. An example could be two family practice physicians practicing in the same location while having different compensation plans. Over time, many HSHs have developed standard plans for their employed physicians. But as described above, these were typically based on individual physician production or performance.
As the industry continues to evolve and move from volume to value, HSHs should review their current physician compensation strategy. Part of this evaluation should include ways to reintroduce group incentives (shared economic interest) into the strategy.
There’s no single best compensation approach. But as you evaluate the right plan for your HSH, there are a few things to keep in mind:
As a starting point, your HSH may want to review the structure of its base individual compensation plan. Many simply establish a base rate per wRVU for each physician specialty and apply that rate to each physician’s wRVUs, which doesn’t reflect the fixed cost economic reality of a physician practice.
A more accurate method would be a tiered system where the rate per wRVU increases with productivity. Here’s a sample of this approach:
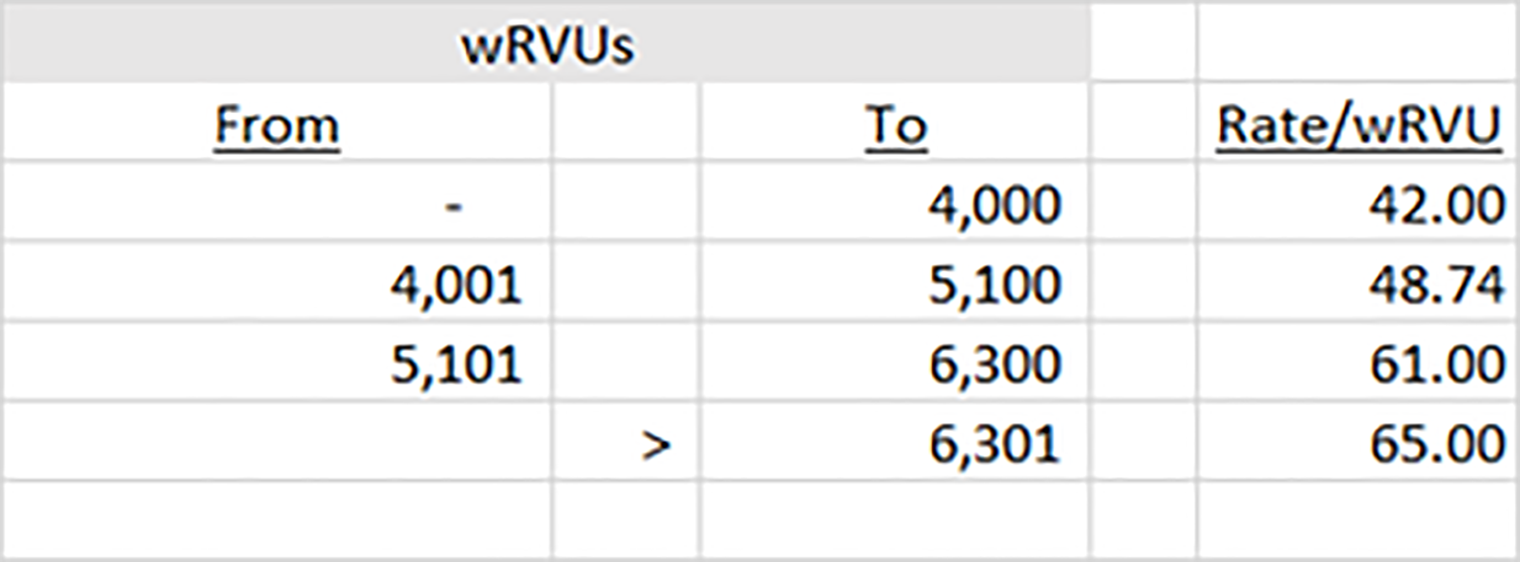
While this doesn’t create a group incentive, it may be a good first step in changing the compensation philosophy to one where increasing levels of productivity result in a higher pay rate.
Next, HSHs should consider adding the group incentive. Again, as a starting point, consider a departmental or location incentive to the rate per wRVU if physicians achieve pre-determined productivity or other goals such as patient satisfaction and quality. This may begin as an upside-only incentive, but eventually should include penalties for unaccomplished goals.
Using the wRVU method above, if a department or location meets its productivity and satisfaction/quality goals, the rate per wRVU increases by X%. Conversely, if the goals aren’t achieved, it decreases the rate by Y%. This ties the economic interests of the department/location providers together and begins to reflect the shared economic interests seen in a private practice.
Eventually, you can expand this incentive/penalty beyond department or location to departments across all locations (e.g., all family practice providers), or throughout the physician enterprise. By extending the approach across the physician enterprise all physicians / specialties have a shared economic interest in the growth and success of the organization.
Most value-based agreements inherently tie the economics of the physician providers together. Gain share, shared risk or full risk agreements are typically enterprise agreements and are measured, paid or penalized at that level. These agreements provide HSHs with an opportunity to incorporate and emphasize group incentives in their physician compensation structure beyond the traditional “volume” incentives.
In broad terms, these value-based agreements will reward the enterprise based on the achievement of cost, clinical quality and patient satisfaction goals. The amount of upside incentives or downside penalties will be determined by the achievement of the quality and satisfaction goals. In other words, if the enterprise achieves its cost targets, but not the clinical or satisfaction goals, the amount physicians receive will be reduced or even eliminated.
These agreements should measure and report the contractual components by physician. Herein lies the opportunity to promote the group incentive by deciding how upside revenues or penalty amounts are distributed to the individual physicians. This can be a much more complicated calculation. However, the design should consider the HSH’s compensation philosophy and strategic plan to include the reimbursement structure for providers that meet cost goals, but not quality or satisfaction goals.
Below is a simplified chart using panel size (member months), cost and quality as the defining metrics. In this example, 20% of the distribution is based on member months, 40% is based on cost and 40% is based on how many of the four quality measures were attained.
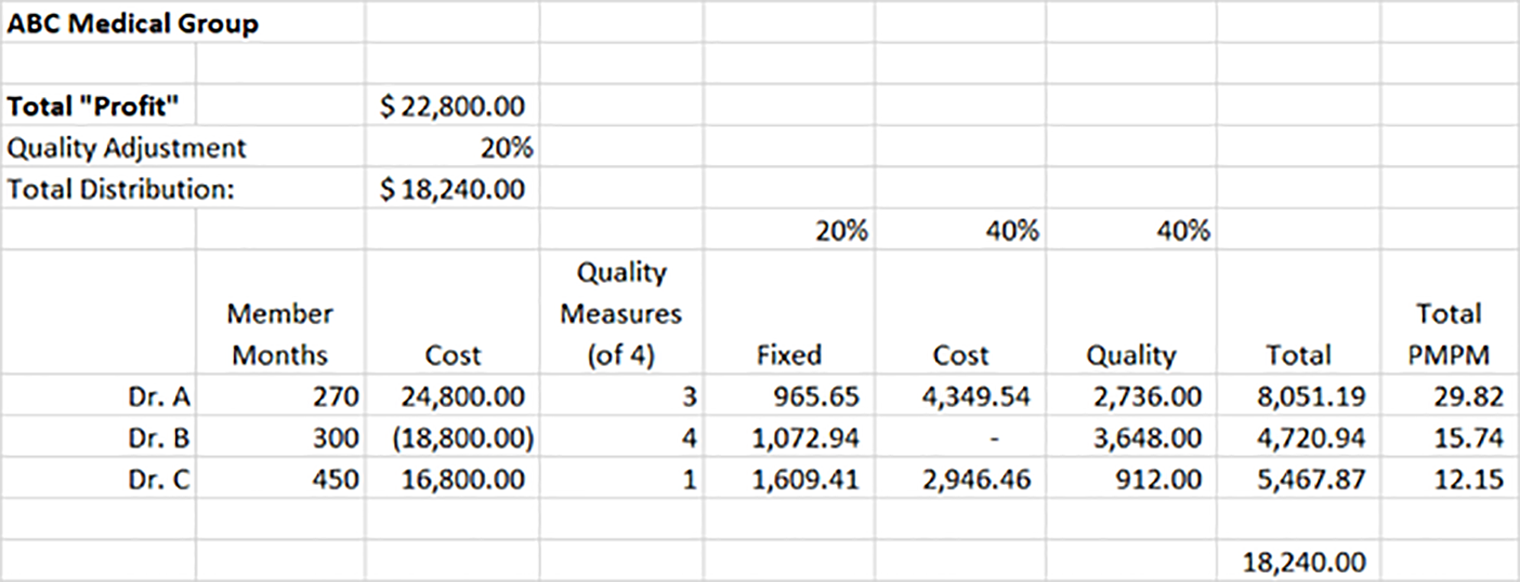
You can see Dr. B had a loss but met all the quality measures, while Dr. C realized a profit but met only one of the quality measures, reducing the overall group distribution. Dr. B received a larger PMPM distribution with a loss than Dr. C, even though Dr. C had a profit but met only one of the quality goals. This model shows a shared economic interest among the providers that’s comprised of multiple measurements, which are in sync with ABC Medical Group’s overarching targets.
For most HSHs individual productivity will continue to drive most of their compensation methodology. After all, fee for service continues to drive most of the physician enterprise revenues. However, combining volume and value-based group incentives can help HSHs create a shared economic interest in their physician enterprise, institute a medical group culture and increase overall performance alignment with the HSH’s strategic plan.
There’s no one-size-fits-all solution to an equitable physician compensation plan. As noted earlier, any physician compensation plan changes should include physician leadership in the design and implementation to be effective. An additional benefit of this approach is enhanced collaboration between administrative and physician leadership to ensure both are working together to achieve the Triple Aim goals — reducing costs, improving quality and increasing patient satisfaction.
If you have any questions about refining your physician compensation plan, contact our healthcare experts.


